Agrammatic/Nonfluent
A problem with the order and production of words, including:
- Effortful speech and reduction in quantity.
- Gradually shorter sentences and words may be left out.
Jump to a section:
Primary Progressive Aphasia (PPA) is a rare neurological syndrome that primarily affects language. Unlike other forms of dementia, the earliest symptoms of primary progressive aphasia are difficulties with speaking, word finding and understanding language rather than memory loss. Adults of any age can develop PPA, though it is most often diagnosed in individuals under 65.
The causes of PPA are linked to underlying brain diseases that damage language networks, most commonly frontotemporal lobar degeneration (FTLD) and, in some cases, Alzheimer’s disease. As the condition progresses, individuals may experience increasing challenges with communication, including word usage, sentence formation, reading and comprehension.
While there is currently no cure, the treatment of primary progressive aphasia focuses on therapies and support strategies that help patients and families adapt. Early and accurate diagnosis of PPA enables tailored care, speech-language interventions, and opportunities to participate in clinical research. At the Mesulam Center for Cognitive Neurology and Alzheimer’s Disease at Northwestern University, our team is at the forefront of advancing PPA knowledge, care and research.
The symptoms of PPA vary depending on the subtype, but all involve progressive loss of language abilities. The three subtypes are:
A problem with the order and production of words, including:
A problem with understanding words, including:
A problem with finding words, including:
What causes Primary Progressive Aphasia?
PPA occurs when harmful proteins accumulate in the brain areas that control language, gradually damaging and killing brain cells.
Most cases are caused by a brain disease called FTLD, while Alzheimer's disease causes the rest.
Learn more about PPA symptoms and causes
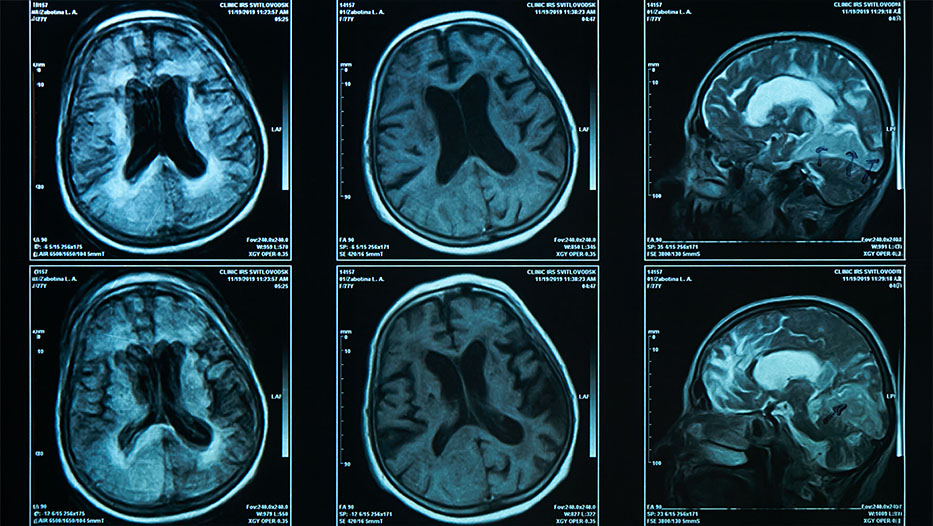
Diagnosing PPA is a complex process of ruling out other conditions, and there is no single definitive test. Instead, clinicians rely on several factors to help identify the underlying pathology.
Diagnosis takes into account:
There is no cure for PPA, but we can often help patients and families maintain quality of life through therapies such as:


Many of our PPA research participants have left behind a unique gift for the Mesulam Center — their artwork. We have compiled a gallery of selected artwork from past and current participants.
Discover how art offers a profound, enduring means of communication and expression amidst language loss.
The Mesulam Center is a global leader in PPA research, with faculty and scientists working to improve diagnosis, identify risk factors, understand disease progression and develop innovative treatments. Find a sample of our research impact in the following studies:
Those living with Primary Progressive Aphasia should consider enrolling in a research program affiliated with the center. Browse our list of ongoing studies recruiting new participants.
